Blood
Blood anatomy and physiology play pivotal roles in cardiac surgery, influencing both the approach to surgical procedures and the management of care during and after surgery. An in-depth understanding of blood's composition and function is essential for optimizing patient outcomes. This detailed examination of blood will cover its primary components, their functions, and their specific relevance to cardiac surgery, including implications for perfusion, coagulation, and inflammatory responses.
Composition of Blood
Blood is a complex, dynamic tissue comprising plasma, red blood cells (RBCs), white blood cells (WBCs), and platelets. Each component serves distinct roles that are crucial during cardiac surgery.
Plasma
Plasma, the liquid component of blood, makes up about 55% of its volume and is primarily water (90%), with the remainder consisting of proteins, electrolytes, nutrients, gases, and waste products. Plasma proteins include albumin, which maintains oncotic pressure and transports substances; globulins, which are part of the immune response; and fibrinogen, which is essential for clot formation. During cardiac surgery, maintaining plasma volume and composition is critical to ensure adequate tissue perfusion and gas exchange.
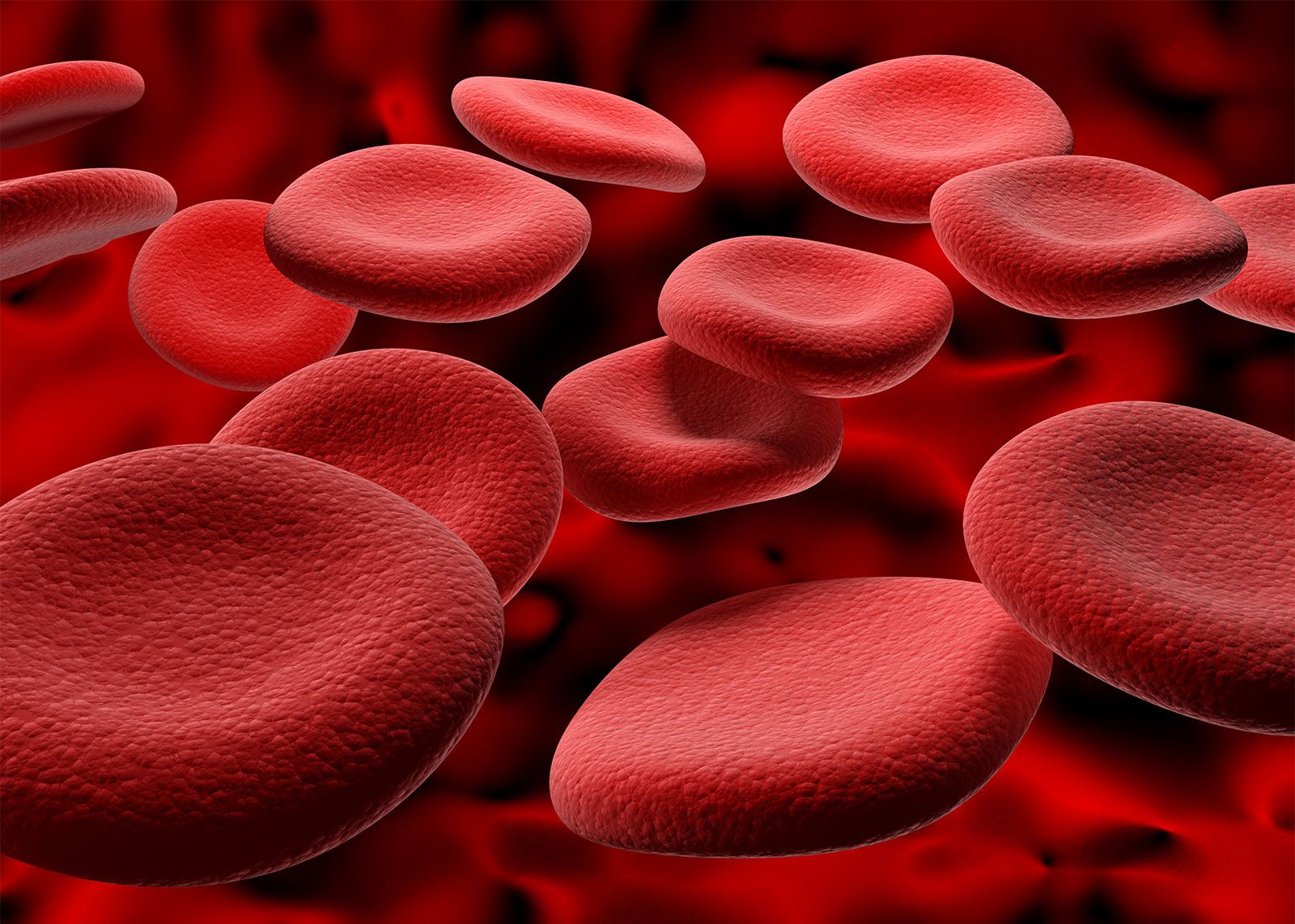
Red Blood Cells (RBCs)
RBCs are responsible for oxygen delivery to tissues and removal of carbon dioxide. They contain hemoglobin, a protein that binds oxygen and carbon dioxide, facilitating gas exchange in the lungs and at a cellular level. In cardiac surgery, preserving RBC integrity and function is vital to prevent hypoxia and maintain organ function.
White Blood Cells (WBCs)
WBCs are key components of the immune response. They protect against infection, a critical concern post-surgery. The major types of WBCs include neutrophils, lymphocytes, monocytes, eosinophils, and basophils, each serving different roles in immune defense and inflammation. Surgical stress can lead to leukocytosis (an increase in WBCs), which needs careful monitoring to differentiate between normal surgical stress response and an infection.
Platelets
Platelets are crucial for blood clotting and hemostasis. They aggregate at sites of vascular injury, forming a plug, and activate the coagulation cascade to stabilize the clot. In cardiac surgery, managing platelet function is crucial to prevent both excessive bleeding and thrombotic complications such as stroke or myocardial infarction.
Physiology of Blood in Cardiac Surgery
The physiological demands of cardiac surgery require precise management of blood's components to address the challenges of perfusion, coagulation, and inflammation.
Perfusion
Effective perfusion, the process of delivering blood to capillary beds in tissues, is essential during cardiac surgery, particularly when using cardiopulmonary bypass (CPB). CPB takes over the function of the heart and lungs during surgery, requiring careful management of blood flow to ensure tissue viability. Maintaining adequate hematocrit levels in the blood is crucial as it affects blood's viscosity and, consequently, its ability to deliver oxygen efficiently.
Coagulation
Coagulation is a significant concern during cardiac surgery due to the high risk of bleeding and thrombotic events. The coagulation cascade involves numerous plasma proteins and is tightly regulated by procoagulant and anticoagulant factors. Surgery and CPB can activate the coagulation system, leading to a hypercoagulable state. Conversely, dilutional coagulopathy can occur from the infusion of fluids and blood products, reducing coagulation factor concentration and impairing clot formation. Managing these opposing risks involves careful monitoring and balancing of coagulation factors and anticoagulants like heparin, which is commonly used during CPB to prevent clot formation in the bypass circuit.
Inflammatory Response
Cardiac surgery, particularly with CPB, induces a systemic inflammatory response characterized by the release of cytokines and other inflammatory mediators. This can lead to complications such as capillary leak, organ dysfunction, and post operative complications like atrial fibrillation or renal impairment. Strategies to mitigate this response include using preoperative medications, optimizing CPB techniques, and careful management of blood components.
Blood Conservation
Blood conservation is a critical aspect of cardiac surgery, aimed at minimizing blood loss and reducing the need for transfusions, which are associated with increased risk of complications such as infection, lung injury, and alloimmunization. Techniques include preoperative optimization of red cell mass, intraoperative blood salvage, and pharmacological agents to enhance coagulation.
Conclusion
The intricate nature of blood's anatomy and physiology has profound implications for cardiac surgery. A deep understanding of how blood components interact and can be manipulated provides a foundation for surgical strategies that improve patient outcomes. Effective management of perfusion, coagulation, and the inflammatory response is essential, requiring a multidisciplinary approach involving surgeons, anesthesiologists, and perfusionists. Advances in surgical techniques, blood conservation methods, and postoperative care continue to evolve, driven by ongoing research into the complex interplay of blood and heart function during and after cardiac surgery.