Coagulation in Cardiac Surgery
Coagulation is a critical physiological process in cardiac surgery, involving a complex cascade of events that leads to blood clot formation to stop bleeding. This process is especially crucial in cardiac operations, where precise control of bleeding is necessary to prevent both excessive blood loss and thrombotic complications.
Overview of the Coagulation Cascade
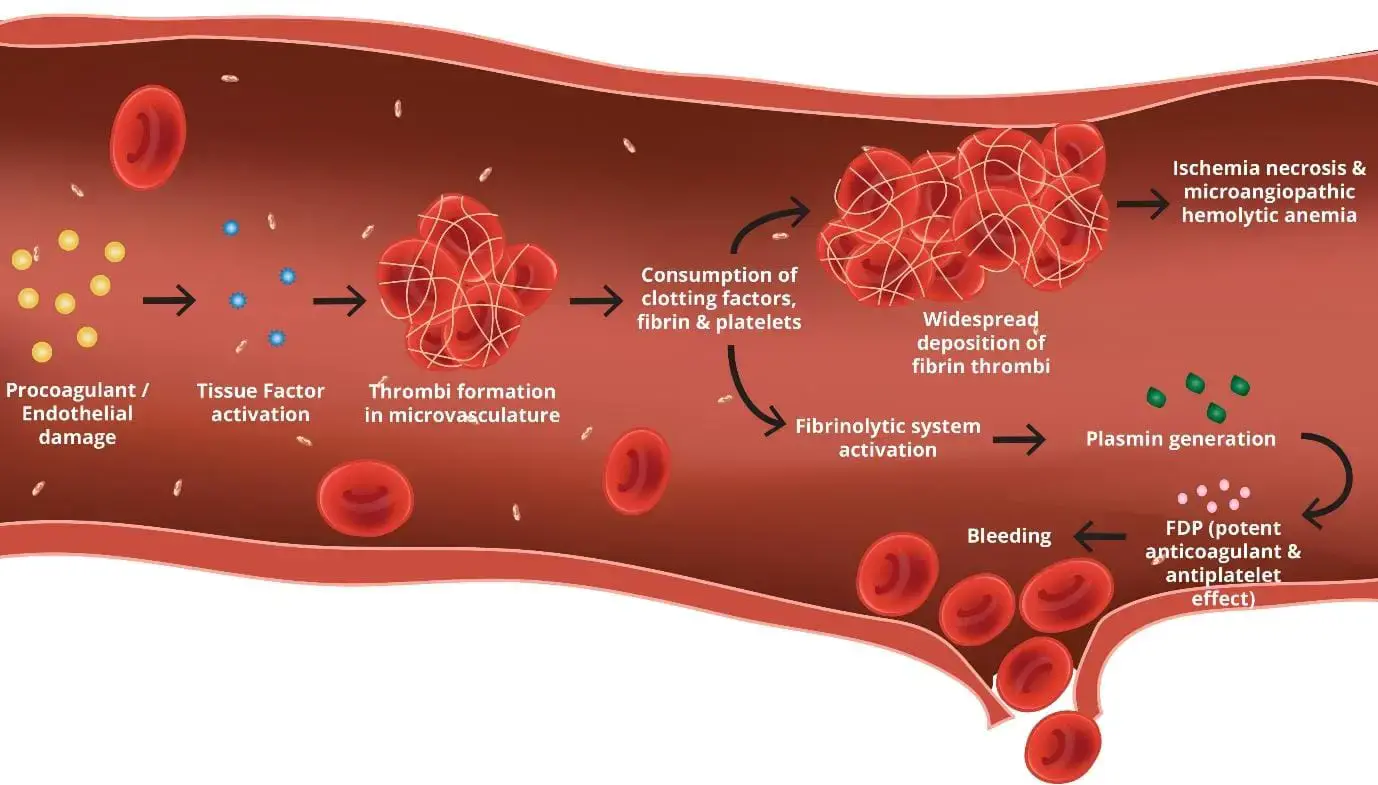
The coagulation cascade is a series of reactions that occur in sequence, involving various clotting factors that are predominantly produced by the liver. These factors are usually present in the blood as inactive precursors, which, when activated, trigger the next factor in the sequence:
- Intrinsic Pathway: Activated by damage inside the vascular system, and involves factors XII, XI, IX, and VIII.
- Extrinsic Pathway: Triggered by external trauma leading to tissue damage and involves tissue factor (TF) and factor VII.
- Common Pathway: Where both pathways converge, involving factors X, V, II (prothrombin), and I (fibrinogen), leading to the formation of a fibrin clot.
Role of Coagulation in Cardiac Surgery
Cardiac surgery poses unique challenges to the coagulation system. The use of cardiopulmonary bypass (CPB) machines, the handling of heart tissues, and the exposure to foreign surfaces during surgery can significantly disrupt normal coagulation processes:
Challenges During Cardiopulmonary Bypass (CPB)
During CPB, blood is exposed to non-physiological surfaces, which can activate coagulation pathways abnormally. Moreover, the dilution of blood with fluids and the cooling and rewarming processes associated with CPB can impair clotting factor functionality, leading to a condition known as coagulopathy:
- Dilutional Coagulopathy: Caused by the dilution of clotting factors and platelets in the blood.
- Hypothermia: Reduces the enzymatic activity of clotting factors and platelet function.
Management of Coagulation
Effective management of coagulation during cardiac surgery requires meticulous planning and intervention:
- Anticoagulation Therapy: Anticoagulants such as heparin are used during CPB to prevent clot formation in the bypass machine. The dosing of heparin is monitored using the activated clotting time (ACT) to ensure it is within a therapeutic range.
- Reversal of Anticoagulation: After CPB, heparin is neutralized with protamine sulfate to restore normal coagulation function.
- Use of Blood Products: Transfusions of fresh frozen plasma, platelets, and clotting factor concentrates may be necessary to manage bleeding associated with coagulopathy.
Conclusion
Coagulation management in cardiac surgery is complex and requires a deep understanding of both the physiological and surgical aspects of coagulation. Surgeons and anesthesiologists must carefully balance the risks of bleeding and thrombosis to ensure optimal outcomes. This involves not only the use of pharmacological agents but also monitoring technologies and protocols designed to adapt to the dynamic changes in coagulation status during surgery.