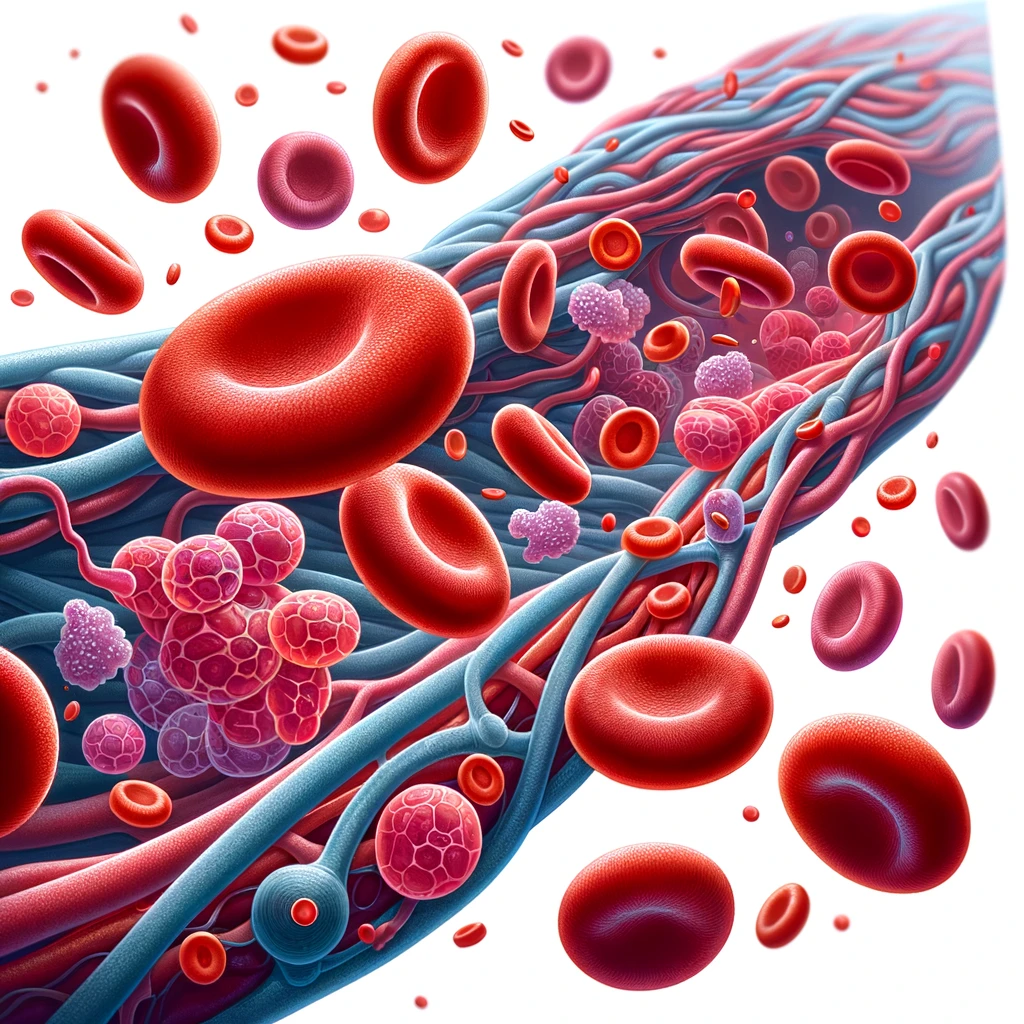
Red Blood Cells
Red blood cells (RBCs) are crucial for the delivery of oxygen to tissues and the removal of carbon dioxide, which is particularly important during cardiac surgery. Their ability to transport oxygen from the lungs to the body's tissues and return carbon dioxide for exhalation makes them indispensable in maintaining physiological balance and supporting organ function during and after surgical procedures.
Composition and Function of RBCs
RBCs, also known as erythrocytes, are the most abundant cells in the human blood. They are primarily designed for gas exchange and have the following characteristics:
- Biconcave Shape: This unique shape increases the surface area for oxygen and CO2 exchange and allows RBCs to deform as they pass through narrow capillaries.
- Hemoglobin Content: RBCs contain hemoglobin, a complex protein that binds oxygen and carbon dioxide. Each hemoglobin molecule can bind up to four oxygen molecules, which facilitates efficient gas transport.
- Lack of Nucleus and Organelles: Mature RBCs do not contain a nucleus or other organelles, which provides more space for hemoglobin and enhances their oxygen-carrying capacity.
Role of RBCs in Cardiac Surgery
During cardiac surgery, the functionality and management of RBCs are of paramount importance due to several factors:
Oxygen Delivery
Maintaining adequate oxygen delivery is a critical concern in cardiac surgery, especially in procedures that involve cardiopulmonary bypass (CPB). CPB can disrupt the normal circulation and oxygenation process, making the role of RBCs even more critical. Ensuring that hemoglobin levels are within an optimal range is essential to support organ function and prevent ischemic complications.
Volume and Viscosity
The volume and viscosity of blood, influenced by the concentration of red blood cells (hematocrit), are important factors in cardiac surgery. Hematocrit levels are a measure of the proportion of blood volume that is occupied by red blood cells. Optimal hematocrit levels are typically between 35% and 40% for most adults, but during cardiac surgery, maintaining a hematocrit level of around 24% to 28% during cardiopulmonary bypass (CPB) is often targeted to balance oxygen delivery with the risk of thrombosis and blood viscosity. A higher hematocrit increases blood viscosity, which can enhance oxygen delivery but also may increase the risk of thrombosis. Conversely, a low hematocrit can reduce blood viscosity, which may improve flow but reduce oxygen-carrying capacity. Balancing these aspects is crucial for the safety and efficacy of surgical interventions.
Another critical parameter in cardiac surgery is the Activated Clotting Time (ACT). ACT is a bedside test used to measure the efficacy of anticoagulation during procedures that involve cardiopulmonary bypass. It is particularly important to ensure that the blood does not begin to clot in the surgical equipment or in the patient's body during surgery. The normal range for ACT is typically around 70 to 120 seconds, but during cardiac surgery, an ACT of at least 400 seconds is maintained when using CPB to ensure sufficient anticoagulation. Monitoring ACT levels helps guide the administration of anticoagulants like heparin and is crucial for preventing coagulation complications during the surgery.
Conclusion
In cardiac surgery, managing the balance of hematocrit levels and ACT is fundamental to maintaining optimal blood viscosity, ensuring effective oxygen delivery, and preventing thrombotic and bleeding complications. Surgeons and anesthesiologists must closely monitor these parameters to adapt to the dynamic conditions during surgery, ensuring patient safety and optimizing surgical outcomes.
Perioperative Management
Perioperative management of RBCs involves monitoring and possibly adjusting their levels through transfusions or other therapies. Anemia is a common issue in cardiac surgery patients and can significantly affect the outcome. Transfusions may be necessary to maintain adequate hemoglobin levels, but they must be balanced against the risks of volume overload, transfusion reactions, and infections.
Conclusion
In cardiac surgery, red blood cells are fundamental in maintaining tissue oxygenation and overall physiological stability. The careful management of RBCs—considering their function, volume, and hemoglobin content—is critical to ensuring patient safety and optimizing surgical outcomes. Surgeons and anesthesiologists must work closely to monitor and adjust the properties of RBCs to adapt to the dynamic conditions during surgery.